What Is Depression, Really?
 It’s normal to experience sadness. (Who didn’t cry when Simba couldn’t wake up Mufasa?) But unlike typical sadness or grief, time can’t and won’t heal Major Depressive Disorder (MDD), the term for clinical depression, which most people just call “depression.” It’s a common mental health condition that shows up like an unwanted houseguest and refuses to leave. This extended period of sadness or emptiness comes with a constellation of other symptoms, like exhaustion, sleep trouble, a shrinking appetite, overeating, sudden crying spells, and sometimes thoughts of suicide. Symptoms range in severity and must last for two weeks or more to receive an MDD diagnosis, though it’s rare than an episode would only last for that short time. Most people have symptoms for six months to a year, and sometimes, they can last for years.
It’s normal to experience sadness. (Who didn’t cry when Simba couldn’t wake up Mufasa?) But unlike typical sadness or grief, time can’t and won’t heal Major Depressive Disorder (MDD), the term for clinical depression, which most people just call “depression.” It’s a common mental health condition that shows up like an unwanted houseguest and refuses to leave. This extended period of sadness or emptiness comes with a constellation of other symptoms, like exhaustion, sleep trouble, a shrinking appetite, overeating, sudden crying spells, and sometimes thoughts of suicide. Symptoms range in severity and must last for two weeks or more to receive an MDD diagnosis, though it’s rare than an episode would only last for that short time. Most people have symptoms for six months to a year, and sometimes, they can last for years.
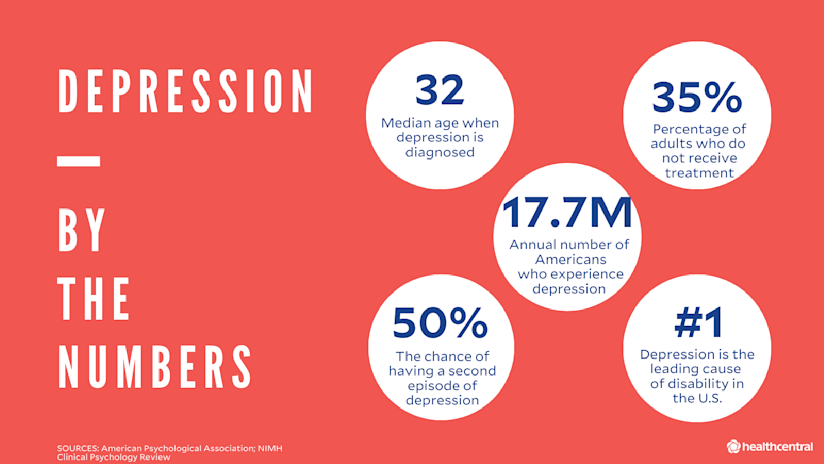
Without treatment, depression won’t fade away on its own. Even if you do white-knuckle it through your first episode of depression, your chance of another recurrence is more than 50 percent. If you’ve had two episodes, that chance shoots up to 80 percent. Meaning, you’re going to want to deal with this sooner rather than later.
One hallmark of depression is an inability to experience pleasure, which is literally no fun. Losing interest in things you once enjoyed often means that your capacity to function at work and home takes a dive. In fact, depression is one of the leading causes of disability in the U.S., as 7.2% of Americans—17.7 million people—experience Major Depressive Disorder, each year.
Other Types of Depression
We talked about MDD (a.k.a. depression) but there are other types of depression. They include:
- Persistent Depressive Disorder. This is a chronic form of depression, formerly known as dysthymia. Sometimes people call it “high functioning” or “smiling” depression. While symptoms aren’t as severe as MDD, they last for two years or longer. People with PDD might feel like they’ve always been depressed. (In cases of “double depression,” people experience severe episodes of MDD within their usual state of chronic depression.)
- Seasonal Affective Disorder (SAD). Depression symptoms start and end seasonally, around the same times every year. Most people get depressed in cold, dark winter, but some people’s mood plummets in summer.
- Premenstrual Dysphoric Disorder (PMDD). Here, depression symptoms are tied to the luteal phase of the menstrual cycle, starting about one week before your period and ending just after your period. Though many of the symptoms mirror PMS—irritability, high anxiety, frequent crying—they’re much more severe. They interrupt your ability to work, destroy personal relationships, and can lead to thoughts of self-harm and suicide. This condition was added in 2013 as a form of depression to the DSM-5, the official guide of mental disorders.
- Peripartum Depression. New mothers with this disorder typically develop symptoms of depression and even psychosis within a few weeks of giving birth. It used to be called postpartum depression and many people still use the term interchangeably. (In some cases, symptoms start during pregnancy; other times, when the baby is several months old—hence the name change.)
- Perimenopausal Depression. In midlife (specifically, the years leading up to menopause), people experiencing this disorder have typical depressive symptoms plus perimenopause symptoms like hot flashes and night sweats.
- Substance/Medication-Induced Depressive Disorder. Substance abuse (alcohol, opiates, sedatives, amphetamines, cocaine, hallucinogens, etc.) or taking some medications, like corticosteroids or statins, can trigger the symptoms of depression. If substance use (or withdrawal from using) is causing your symptoms, you may have this version of depression.
- Disruptive Mood Regulation Disorder. A child with this juvenile disorder is grumpy and bad-tempered most of the time. They have severe, explosive outbursts with parents, teachers, and peers several times a week. Their overreactions are extreme and inconsistent with their developmental level.
Depression strikes people at a median age of 32, but it’s important to remember that depression can happen to anyone, at any age, of any race, gender, or political affiliation. One out of every six adults will experience depression at some time in their life. Fortunately, depression is treatable. That’s why, at the first hint of symptoms, it’s important to make an appointment with a mental health professional who can help determine whether you have depression, and if so, which type—and most importantly, which treatment is appropriate for you.
What Causes Depression?
You’re not going to like this answer, but no one knows for sure. That said, for the past few decades, the prevailing theory is that depressed people have an imbalance in their brain chemistry—more specifically, low levels of neurotransmitters like norepinephrine, epinephrine, and dopamine, which help regulate mood, sleep, and metabolism. We now know it’s a little more complicated than that.
Certain circumstances put people at a higher risk of depression, including childhood trauma, other types of mental illness and chronic pain conditions, or a family history of depression, but anyone can get depressed.
Scientists informed by decades of research believe that the following factors also up your risk of becoming depressed, but they can’t prove causality. Still, they can play heavily in the development of depression, so it’s important to be aware of them:
- Genetics. Research shows that having a first-degree relative with depression (a parent, sibling, or child) makes you two-to-three times more likely to have depression tendencies.
- Traumatic life events from childhood, such as abuse or neglect.
- Environmental stressors, like a loved one’s death, a messy divorce, or financial problems.
- Some medical conditions (e.g., underactive thyroid, chronic pain). Per science, the relationship between these physical conditions and depression is bidirectional, so there’s a chicken-or-egg thing going on because they feed each other.
- Certain medications, including some sedatives and blood pressure pills.
- Hormonal changes, like those that come with childbirth and menopause.
- Gut bacteria. There has been a link established between the microbiome and the gut-brain axis, but it’s only just starting to be studied.
Do I Have the Symptoms of Depression?
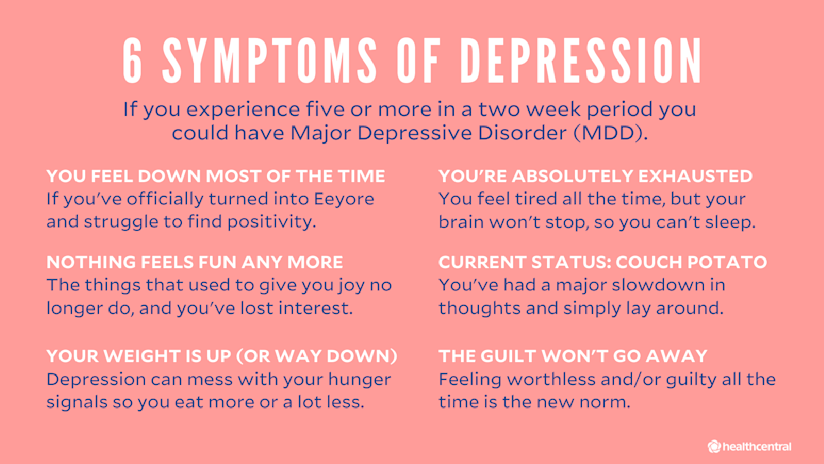
Wondering whether your feelings qualify for clinical depression? Those with MDD experience five or more of the below symptoms during the same two-week period, and at least one must be depressed mood or loss of pleasure. The symptoms would be distressing or affect daily functioning.
- You feel down most of the time.
- The things you liked doing no longer give you joy.
- Significant weight loss (without dieting) or weight gain or feeling consistently much less hungry or hungrier than usual.
- Having a hard time getting to sleep and staying asleep or oversleeping.
- A molasses-like slowdown of thought, becoming a couch potato, or spending days in bed. (This should be noticeable to others, not just subjective feelings of restlessness or slothiness.)
- So. So. Tired. You’re so exhausted you can’t even.
- Feeling worthless a lot of the time, even if you haven’t done anything wrong.
- Being super distracted, indecisive, and unable to concentrate.
- Recurrent thoughts of death or suicide(with or without a specific plan to actually do it). If you need help for yourself or someone else, please contact the National Suicide Prevention Lifeline at 1-800-273-TALK (8255).
How Do Doctors Diagnose Depression?
When you’re having a depressive episode, it might feel like you’re destined to feel terrible forever. That’s not true. It’s just what your depressed brain wants you to think. The hardest step is ignoring that feeling and making an appointment with a doctor and/or mental health professional, such as a psychologist or psychiatrist. A mental health professional is the only expert that can help you figure out if you are depressed.
Unfortunately, there’s no easy blood test that can determine if you have depression, though that would make diagnosis a lot easier. (Get on it, science!) The DSM-5 helps clinicians make that call with a targeted list of common symptoms. To be diagnosed with MDD, patients must experience five or more of the above symptoms (see “Do I Have the Symptoms of Depression?”)—one must be depressed mood or loss of pleasure—during a two-week period.
Even if your symptoms match up to MDD, though, your doctor should rule out any underlying medical causes first. Some conditions, such as thyroid disease and vitamin deficiency, can mimic symptoms of depression. Next, consider any medications you’re currently taking.
If this sounds like you or someone you know, make an appointment with a mental health professional. Now. Don’t wait! What’s the worst thing that can happen? If you feel better by the time the appointment rolls around, you can always cancel it. If you don’t, you’ve saved yourself precious time (and unnecessary pain) by taking steps to managing your mental health.
What Are the Best Treatments for Depression?
Regardless of why you’re depressed, it’s important to get treatment before the condition starts to erode your quality of life. Studies and surveys show that most adults in the U.S. who screen positive for depression remain untreated. Don’t be one of them.
As scientists continue to hash out theories about the root causes of depression, research shows that the most effective treatment is a mix of psychotherapy, medication, and lifestyle changes. It might take a (frustratingly long) while to find the right recipe —antidepressants work differently in different people so finding the right fit often takes some trial and error. Plus, the mental health professional you’re working with will be by your side. They won’t give up and neither should you. Some of the treatment options available are:
Psychotherapy
This doesn’t mean you’ll find yourself reclined on a couch, complaining about your relationship with your mother (though it might). A psychiatrist, psychologist, therapist, or licensed clinical social worker might use a variety of techniques to help change the negative thinking, beliefs, or behaviors that exacerbate your depression and make your world seem hopeless. Types of therapy include psychodynamic therapy, Cognitive Behavioral Therapy (CBT), and interpersonal therapy.
Medication
*WARNING – TRY EVERYTHING BEFORE YOU TRY MEDICATION. YOU COULD LOOSE YOUR JOB, AND MAKE IT MORE DIFFICULT TO GET ANOTHER ONE. ALSO, YOU WILL HAVE TO TURN IN ALL YOUR GUNS, YOU CAN NOT WORK WITH CHILDREN AND MANY OTHER RESTRICTIONS NOW APPLE.
Your depression might require more than coaching. Doctors may prescribe medication including antidepressants, mood stabilizers, and/or antipsychotic pills in order to decrease the symptoms of depression. These include:
- SSRIs (selective serotonin reuptake inhibitors) like Prozac (fluoxetine), Paxil (paroxetine), and Zoloft (sertraline) and SNRIs (serotonin and norepinephrine reuptake inhibitors) like Cymbalta (duloxetine) and Effexor XR (venlafaxine) make neuro-transmitters serotonin and norepinephrine already existing in the brain more available.
- TCAs (tricyclic antidepressants) like Tofranil (imipramine) and Norpramin (desipramine) and MAOIs (monoamine oxidase inhibitors) like Emsam (selegiline) and Marplan (isocarboxazid) are first-generation antidepressants that work similarly on neuro-transmitters, but they’re used less often because of unpleasant side effects.
- Doctors may also use atypical antidepressants like Zyban or Wellbutrin (bupropion) or Remeron (mirtazapine) that affect serotonin, norepinephrine, and dopamine levels in ways unique from other anti-depression drugs. Or they may add atypical antipsychotics, a.k.a. second-generation antipsychotics like Seroquel (quetiapine) or Abilify (aripiprazole). They’re “atypical” in that they affect dopamine and other neurotransmitters without the physical side effects, such as tics and tremors, that first-generation antipsychotics can cause.
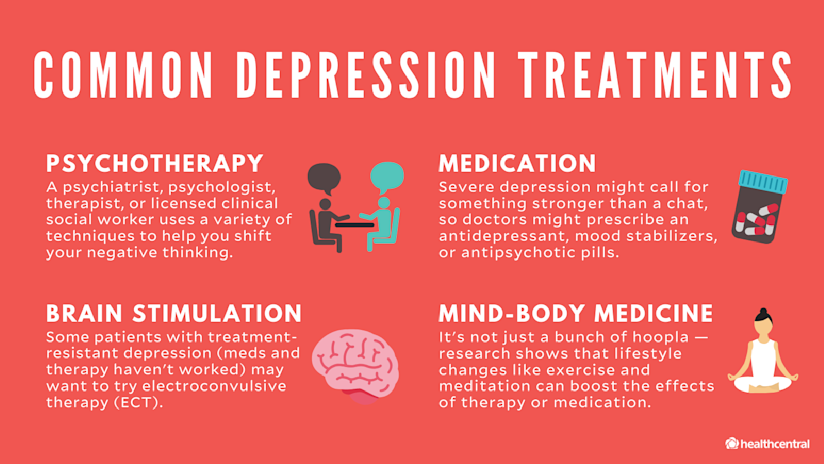
Brain Stimulation
For treatment-resistant depression that doesn’t get better after exhausting psychotherapy and more than two classes of antidepressants (such SSRIs and TCAs), there are more hardcore options. Severe depression may warrant electroconvulsive therapy (ECT), which you might remember from One Flew Over the Cuckoo’s Nest. Fear not—modern ECT is safe, performed under anesthesia, and much less aggressive than you see in the movies.
There is also repetitive transcranial magnetic stimulation (rTMS) which some docs refer to as “ECT Lite”. For severe depression, some people receive vagus nerve stimulation (VNS), a surgical implant that works kind of like a pacemaker, sending electric pulses to the brain.
Other Treatment Approaches
These may include:
- For severe, treatment-resistant depression, the FDA recently approved esketamine, a nasal spray based on the party drug/anesthetic ketamine. Experts say it works by kicking up production of glutamate, a neurotransmitter that helps prompt the brain to form new neural connections.
- Sadness during seasonal depression (SAD) can be alleviated with melatonin-regulating light therapy.
- Postpartum depression may be treated with Brexanolone (Zulresso), an IV version of the body’s own neurosteroid allopregnanolone.
- Research shows that lifestyle changes like incorporating exercise and mindfulness can amplify results of medication and therapy. Even if they aren’t foolproof mood-lifters, it never hurts to build a health-supportive routine.
Where Can I Find Depression-Related Communities?
The thing about depression is that it makes you want to roll yourself into a blanket burrito and never come out. But shutting out the world can make an already-bad situation worse by giving you free reign to neglect your needs, ruminate over your perceived flaws, and destroy any chance of forward momentum. Along with therapy and medication, finding supportive people—and connecting with them online and in real life—is a key part of taking care of yourself. Here’s where to start.
Top Depression Instagrammers and Bloggers
- Tonya Ingram, @tonyainstagram, tonyaingram.com
Follow because: She has one hell of a way with words—after all, she is a poet and author. She also battles some pretty heavy stuff like depression, lives as a “lupus legend” (her words—we love) and is currently waiting on the sidelines for a kidney transplant. She takes it all day by day and shares how she gets out of bed, looks herself in the mirror, and figures out how to simply… survive.
- Scott Ste Marie, @depressiontoexpression, depressiontoexpression.com
Follow because: Immediately, he sounds like someone you want to be friends with, someone whose vibe you want to channel. A former Twitter employee and now public speaker, Scott isn’t going to guide you on some path to a complete cure—nor is he going to sugarcoat the realities of living with depression. In order to overcome your demons, Scott believes you have to come to terms with the fact that sometimes life sucks, and that’s okay.
- Kevin Hines, @kevinhinesstory, kevinhinesstory.com
Follow because: You know the saying “What doesn’t kill you only makes you stronger”? Kevin Hines is living proof. He is the only person ever to survive a suicide attempt from the Golden Gate Bridge. After a sea lion kept him afloat, he was reborn as someone who now devotes his life to making sure you’re here tomorrow—which is why he regularly uses the hashtag #beheretomorrow.
- Lola, Gina, and Nora Tash, and Nicole Argiris, @mytherapistsays, mytherapistsays.ca
Follow because: Sometimes the only way to come out of a deep dark hole is with the universal language of laughter. These girls (mostly family or like family) create endless hilarious memes that represent the real trials and tribulations of living in today’s social media-infested world. The point of it all? So you know that, as they put it, “you’re never alone and never as batshit as you think.”
- Sad Girls Club, @sadgirlsclub
Follow because: It’s not your typical reel of inspirational quotes and nod-worthy memes — though, those are sprinkled in, too. Mostly, this feed—run by women of color (including founder @elyse.fox)—gives you actual advice on how to cope with depression, especially in modern-day situations, like discussing mental health at work (hashtag awkward). This feed gives you the ammo you need to shut down stigma.
- Kate Allan, @thelatestkate
Follow because: Animals make everything better — especially when they’re paired with a quirky drawing and an all-too-familiar feeling. A wolf that speaks to your soul; a fox that gives you all the feels; and a bird who tells it like it is. Run by artist, author, and anxious human Kate, this page (and the cute animals that live there) is a feel-good must-follow.
- The Sad Ghost Club, @theofficialsadghostclub, thesadghostclub.com
Follow because: Nathan, Lize, and Helen are besties—or, ghosties, as they refer to themselves—who came together to share life with mental illness from behind the computer screen. These ghosts don’t sugarcoat things, but they’re also not gloom and doom. You’ll be hooked on their graphics and positive (but not overly earnest) messages.
Top Depression-Related Podcasts
- The Hilarious World of Depression. Stand-up comedy meets a psych appointment when actors and comedians struggling with depression tell their (surprisingly funny) mental health stories to “professionally depressed” host John Moe.
- Terrible, Thanks for Asking. Author Nora McInerny, who has dealt with depression, isn’t afraid to ask the awkward questions, as real listeners share their own tales of coping with grief, despair, and anxiety.
- Jen Gotch is OK…Sometimes. Ladyboss CEO and ban.do founder Jen Gotch gets vulnerable and real every week, sharing her struggles with mental health.
- Happier with Gretchen Rubin. It’s no surprise that the author of The New York Times bestseller The Happiness Project has tons of suggestions to help you emerge from your sad cave, build positive habits, and create a happier outlook. Her slightly skeptical sister Elizabeth Craft keeps all that sunshine in check.
- Anthologies of Hope. You’re here, and you’re reading this, so that in itself proves that you haven’t given up hope. But it’s not just that you are here—it’s why you’re here. This podcast dives even deeper into that “why” and tries to bring that to the forefront of your mind instead of the other garbage trying to pull you down. Host Rick Osowski, who has battled depression, brings a variety of guests into the fold to talk about their why.
Top Depression Support Groups and Non-Profits
- Anxiety and Depression Association of America (ADAA). This nonprofit is dedicated to the prevention, treatment, and cure of anxiety, depression, OCD, PTSD, and co-occurring disorders. Come here for new research, monthly webinars from mental health experts, educational infographics and stats, and a Find-a-Therapist database you can search by disorder. You can always find (free) support on the ADAA Online Peer-to-Peer Support Group or support group iOS app for iPhone.
- National Alliance on Mental Illness (NAMI). This nonprofit mental health advocacy group offering free education and support programs such as NAMI Peer-to-Peer (eight free sessions for adults with specific mental health conditions). You can also connect with other folks who have depression on this org’s online message boards and via NAMI Connection (use the site to find a weekly or monthly recovery group near you).
- Reddit, r/depression. Reddit is the hideously under-designed social website for anonymous users with a bad rep for attracting “incels” and “neckbeards.” The self-proclaimed “Front Page of the Internet” has memes, conspiracy theories, and thousands of communities called subreddits—and some of them are quite lovely. For example, the r/depression subreddit is over a decade old with more than half a million subscribers. In here, the vibe is all about empathy, support, and helpful feedback. (A recent study even found that visiting the subreddit caused a “positive emotion change” in users.)
- Talkspace. More like “safe space.” It’s online, it’s private, and it’s “open” 24/7. Over 1 million people use Talkspace to get matched up with one of their 5,000+ licensed therapists and then message them…as much and as often as they’d like. There are different packages depending on your needs, but the instant feedback and comfort is pretty much priceless.
- Sad Girls Club. This is a nonprofit, an online community, and an Instagram handle (see above) focused on the millennial and Gen Z experience of mental illness (depression, anxiety, or something undiagnosed all count). They host meetups IRL where you can connect with similar people and try a cool twist on art therapy like a poetry slam or embroidery class.
- To Write Love on Her Arms (TWLOHA). It’s not just a nonprofit — it’s a movement. Online, at in-person events, through social media and blogs, TWLOHA creates a place for hope and healing through depression, addiction, self-injury, and suicide. People who attend their events and join this community have said they’ve felt transformed. Worth a try, yea?
-
We are in this Together!
-People Start to Heal The Moment They Are Heard-Health and Wellness Associates
EHS Telehealth
DR MARK WILLIAMS MD BC-PSYCH



